Culturally Competent Interprofessional Education and Тrаining Strategies to Reduce Health Disparities and Improve Patient Sаtisfасtion in Underserved Minority Communities
Culturally Competent Interprofessional Education and Тrаining Strategies to Reduce Health Disparities and Improve Patient Sаtisfасtion in Underserved Minority Communities
Emily Smedek, Ashley Do, Anna Foust, Tiffany Johnson, and Christina Williams
UNC Charlotte School of Nursing, Graduate Nursing Program Student (MSN, DNP, PhD)
Abstract
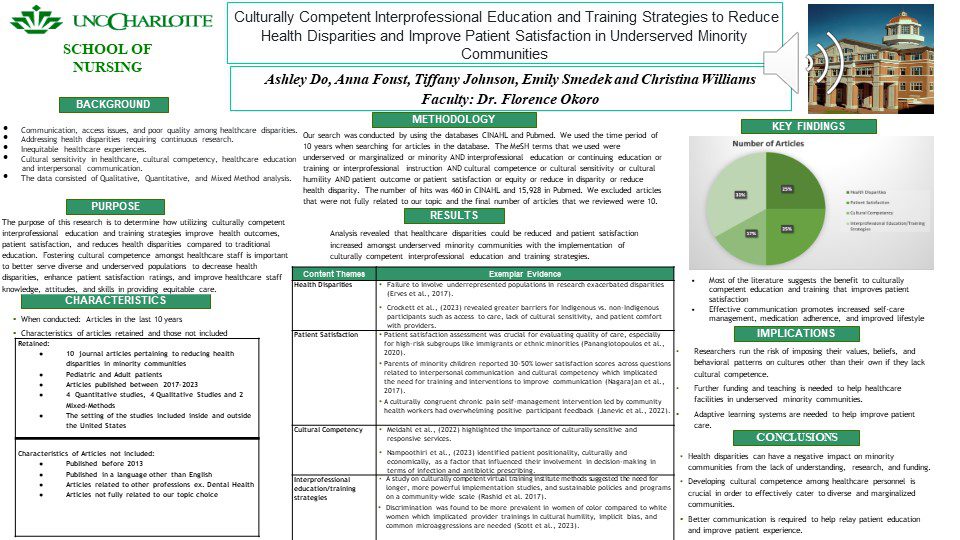
Purpose: To determine how utilizing culturally competent interprofessional education and training strategies improves health outcomes, patient satisfaction, and reduces health disparities compared to traditional education. Fostering cultural competence amongst staff is important to better serve diverse populations.
Background:
- Communication, access issues, and poor quality among healthcare disparities
- Addressing health disparities requiring continuous research.
- Inequitable healthcare experiences.
- Cultural sensitivity, competence, education and interpersonal communication in
healthcare. - Data consisted of Qualitative, Descriptive, Cross-sectional, and Mixed Method analysis.
Methods: This was a systematic review
Results: Electronic databases were searched to locate primary research studies about underserved minority communities and the effects of culturally competent interprofessional education and training strategies on reducing health disparities and improving patient
satisfaction. 10 studies met the inclusion criteria and were extracted and analyzed. The findings of the systematic review showed a need for healthcare clinicians to participate in cultural competency training in order to minimize treatment disparities among racial and ethnic groups.
Conclusion: Patient-oriented medical promotions and research identified barriers related to underserved minority populations’ access to care and communicative effectiveness resulting in efforts to enhance preventative healthcare strategies. There is a need for healthcare clinicians to participate in competency training with the implementation of evidence-based research in order to minimize disparities in underserved communities.
Keywords: Underserved or marginalized or minority AND interprofessional education or continuing education or training or interprofessional instruction AND cultural competence or cultural sensitivity or cultural humility AND patient outcome or patient satisfaction or equity or reduce in disparity or reduce health disparity.
Presentation
Biography
Emily Smedek, BSN, RN
Emily Smedek is a FNP student at the University of North Carolina at Charlotte. She graduated from Wingate University with a Bachelor’s in Biology and a minor in Psychology and went on to pursue her ABSN from Northeastern University. Since obtaining her nursing degree she has been working in an Emergency Department.
Christina Williams, BSN, RN
Christina Williams is a FNP student at UNC Charlotte with a 7-year background in ER nursing currently working as a Care Advisor remotely while pursuing her degree.
Tiffany Johnson, BSN, RN
Tiffany Johnson is a FNP student at the University of North Carolina at Charlotte. She graduated from Foothills Nursing Consortium where she obtained her Associate degree in Nursing and then went on to obtain her Bachelor of Science in Nursing from Western Carolina University. She has 20 years of experience in nursing with a background in Long Term Care, Hospice, Ltach, Med-Surg, Post-Surgical, and Orthopedics. She is currently working in Long-Term care as a Charge Nurse while pursuing her degree.
Ashley Do, BSN, RN
Ashley Do is an FNP Master’s student at the University of North Carolina-Charlotte. She graduated from Wake Technical Community College with her Associate in Nursing and went on to receive her Bachelor of Science in Nursing at the University of North Carolina-Wilmington. She has a background in the Surgical/Trauma Intensive Care unit in Durham, North Carolina. Anna Foust is a FNP student at the University of North Carolina at Charlotte. She graduated from Clemson University with a Bachelor of Science in Nursing. She has 5 years of nursing experience in Cardiac ICU, Emergency Department, and Infusion. She is currently working in pre-op and PACU while pursuing her degree.
Faculty Committee Advisor(s)
Florence Okoro, PhD, RN